PRE2023 1 Group2
Dining Monitoring Device for Patients with Mild Dementia
Group members
| Name | Student ID | Department |
|---|---|---|
| YooungGi Park | 1534718 | Computer Science and Engineering |
| Zabiollah Amiri | 1522175 | Electrical Engineering |
| Thomas Paul Smids | 1684329 | Computer Science and Engineering |
| Rune Bal | 1755897 | Biomedical Engineering |
Introduction & Problem Statement
Maintaining a healthy and balanced diet is essential at every stage of life[1], but it takes on even greater significance as we age. For our elderly population, proper nutrition becomes a vital cornerstone of well-being, impacting both the quality of life and overall health. As we age, our nutritional needs change, and we need to pay special attention to the foods we consume. However even a well-balanced diet can be insufficient in case of improper food intake.
In our elderly population forgetfulness, and diseases like Dementia, especially Alzheimer's[2] can really impact proper food intake. This could for example lead to skipping these essential meals, or conversely eating to much as a consequence of forgetting that one has eaten before.
The device we will be developing will be one that helps elderly people suffering from Alzheimer’s disease with finishing their meal. Research shows that 37.3% of people with mild Alzheimer's have difficulty keeping attention while eating. This is still relatively low compared to people with severe Alzheimer's, where 83.7% has trouble finishing a meal because they get distracted.[3] But because almost all people with severe Alzheimer's live in assisted home, our decision is to look at the group of people with mild Alzheimer's. The reason for this is that people with severe Alzheimer's not only are easily distracted, but also have motor function impairment and other cognitive impairments which make them incompatable with our device. In the mild stage, these symptoms are considerably less so therefore our product is more suited for this user group.
Milestones
Phase 1 Subject Research
- Find Subject
- Literature studies
- Identify problem and objective of the project
- Who are the users?
- What do they want?
- Is there existing solutions to the problem? state-of-the-art research
Phase 2 Design
- Conceptual design
- Come up with multiple designs for the subject, identify strength and weakness of each design, and analyze key aspects for the product.
- Build initial design
- Requirements review
- Identify functional/non-functional requirements.
- Identify MSCW(MoSCow method).
- Be more specific for software design.
- ex) “The device should ring when the signal is on within x seconds”.
- Identify technical requirements
- Identify which skills will be required
- Programming language.
- Soldering
- Required resources
- What are the components needed to build the product?
- Identify which skills will be required
- Identify functional/non-functional requirements.
- Final design concept
- Based on findings from the requirement review, we create final design concept for the next phase.
Phase 3 Build and implementation
- Concept drawing or First design using CAD
- Software design
- Based on Requirement review from Phase 2.
- Hardware design
- Based on Final design concept.
Phase 4 First prototype, test and evaluation
- Finish first prototype
- Testing
- Test individual components.
- Test software and hardware combined.
- Survey
- Discover a more in depth individual user needs.
- Evaluate results
- Check the quality of the product.
- See if there is improvements that can be made within the given time.
Phase 5 Final Documentation
- Final presentation/ video/ discussion
Approach / Planning
Every monday at 9:30 a tutoring session will take place. After that an in-person meeting will take place. If the need arises for anymore meetings, they will be scheduled. Further communication will be done through a whatsapp group.
| Week | Task | Associated Milestone | Name | |
|---|---|---|---|---|
| 1 | Planning & Set-up | Pre- | Everyone | |
| 1 | Literature Research | Phase 1 | Everyone | |
| 2 | Continue Research | Phase 1 | Everyone | |
| 3 | State of the Art | Phase 1.2, 2.1 | Rune | |
| 3 | Functional requirements | Phase 1.2, 2.1 | Bryan | |
| 3 | Further Literature Research | Phase 1 | Zabiollah, Thom | |
| 3 | First Conceptual Design | Phase 2.1 | Zabiollah, Bryan | |
| 4 | Face Tracking Algorithm research | Phase 2 | Thom | |
| 4 | Research Attention Grabbing Stimulus | Phase 2 | Rune | |
| 4 | Second Conceptual design | Phase 2.1 | Everyone | |
| 4 | Component/Sensor List | Phase 2/3 | Zabi | |
| 4 | Sketch of concept | Phase 2/3 | Bryan | |
| 5 | Order and familiarize with circuit | Phase 2/3 | Zabi | |
| 5 | Familiarize with Software PYNQ board | Phase 3 | Bryan | |
| 6 | Coding for PYNQ to activate actuators | Phase 3 | Bryan | |
| 7 | Testing with users | Phase 4 | Everyone | |
| 7 | evaluate results | Phase 4 | Everyone | |
| 7 | prepare presentation | Phase 5 | Everyone | |
| 7 | Finish first prototype | Phase 4 | Everyone | |
| 8 | Finish / Improve parts if not complete | Phase 4 | Everyone | |
| 8 | Finish edit wiki | Phase 4 | Everyone |
Requirements
Functional requirements
Several issues that hinder independent eating experience in dementia patients of all levels have been identified through paper research. We came up with functional requirements to encounter some of these difficulties in this section. These functional requirements are characteristics that must be implemented in our product in order for patients/users to effectively use the product and increase the above-mentioned quality of autonomous eating experience.
To begin, it is critical to consider features in terms of user experience, particularly for elderly people with dementia. Functions such as ease of use (simplicity), ease of access, user-friendliness, intuitivity, and safety measures must be the baseline of features to be considered while designing the product.
- Difficulty in proper use of utensils
- Difficulty in scooping the proper amount of food
- Difficulty in recognizing the total amount of food provided
- Difficulty in maintaining attention while eating
- Difficulty in maintaining alertness while eating
The above problem characteristics were discovered in a well-known academic research paper that has been cited over 100 times.[4] However, due to the course's time and resource constraints, we have mostly focused on the last two problems, which are the Difficulty maintaining attention/alertness while eating. The followings are the functional requirements for our device to tackle the problem.
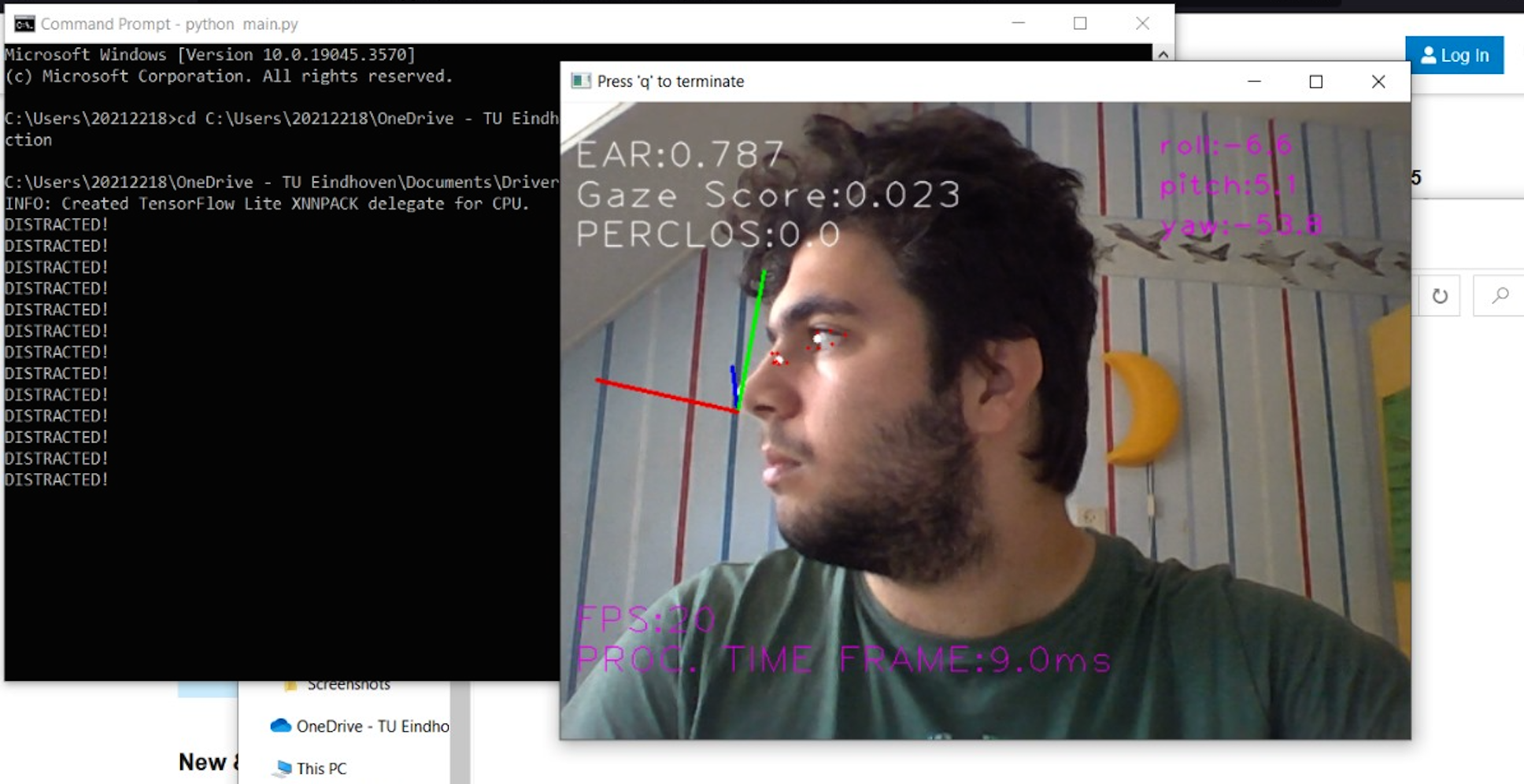
- The product should have activity tracker or camera sensor to detect users face movement
- The product should have visualization actuators to engage with the users
- The product should provide audition actuators to engage with the users
- The product should have software to detect user's alertness
- The product should activate the components when the user's alertness is declining
- The product should positive feedback to users during eating for them to staying in focus
- The product should include features to minimize distraction in the environment
Further research should be carried out to finalize or improve these guidelines, and surveys or usability testing with users would provide valuable feedback to develop these requirements and create a higher quality product that meets their demands.
MoSCoW
In this section the requirements of the product will be specified, using the MoSCoW method. Meaning the requirements of our product are sorted into 4 categories: Must have, Should have, Could have and Won't have.
1. Must have
- Retrieve and record data concerning the users attention.
- Have visual and sound cues to regain attention of the user.
- Easy to use system/controls.
- Easy to set up and move.
2. Should have
- A long battery life or support for an electronic device with long battery life.
- Have an intuitive alert system.
- If any, have an intuitive UI (User Interface).
- Be physically robust.
3. Could have
- Retrieve data concerning other basic medical information, such as blood pressure, hydration level.
- Report conclusions about the data to a Doctor or responsible person.
- Be able to compare user nutrient intake to their recommended intake.
4. Won't have
- Be able to retrieve data concerning advanced medical information, such as amount of various vitamins or various ions.
The above requirements are not final and can still be changed during the process.
Users
User Profile
In this section, we will provide a detailed profile of the users of the our device. Understanding needs, and challenges of our target users is essential for designing our device.
1. Demographics
- Age: The typical age range of people with Alzheimer's disease who will use our device varies but is generally older adults. The primary users are typically aged 65 and older. We are focussing on elderly in the middle stage of Alzeimer's, and not in the early or late stage. Because the age range and development of Alzheimer's differs extremely from peron to person we keep our age range of 65 and older.
- Gender: Alzheimer's disease affects both males and females, with no gender-specific considerations impacting device usage.[5]
2. Medical Condition
- Alzheimer's disease: Users of the device are likely to have varying stages and severities of Alzheimer's disease. The users we foccus on are in the middle stage. These patients cope with symptoms like memory loss, confusion, disorientation, difficulty with decision-making, reduced motor functions and difficulty maintaining attention. Challenges include medication management, food intake, and recognizing the need for medical attention.[6]
3. Cognitive Abilities
- Cognitive impairment: The extent of cognitive impairment in our user group can range from mild to severe. Some users will experience difficulty in understanding and operating complex devices. Therefore the device should be simple, work with clear visual and sound cues, and need minimal user input so that the device can be used effectively.
- Memory loss: Memory loss is a common symptom of Alzheimer's disease. Users may have difficulty recalling recent events, which can impact their ability to remember device usage instructions and data generated by the device.
4. Caregiver
- Involvement of caregivers: Caregivers play a vital role in assisting users with Alzheimer's disease. They may be responsible for device setup, maintenance, and interpretation of data. But since we focuss on people in the mild state of Alzheimer's we can expect most of our users to live at home with minimal assistance. So the device should be easy useable by the user and should not need the help of a caregiver.
5. Daily Activities
- Daily Routine: Users often follow predictable routines, and the device should easily integrate into their daily activities.
Initial conceptual design
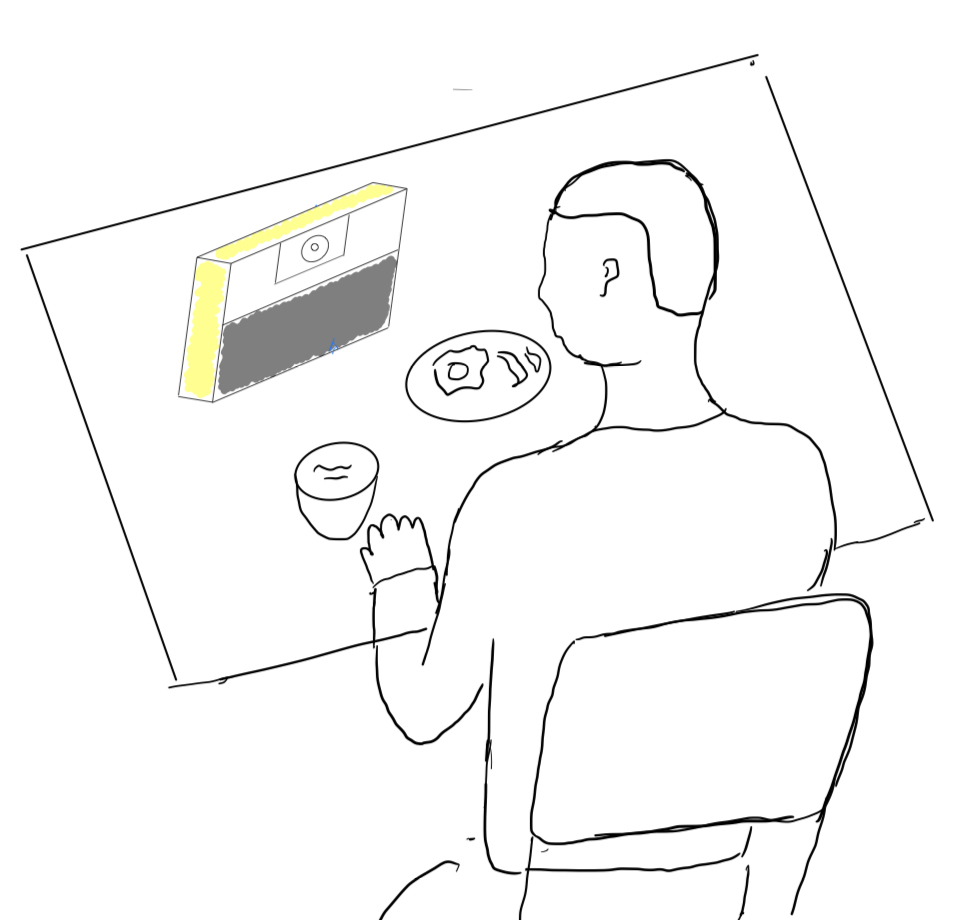
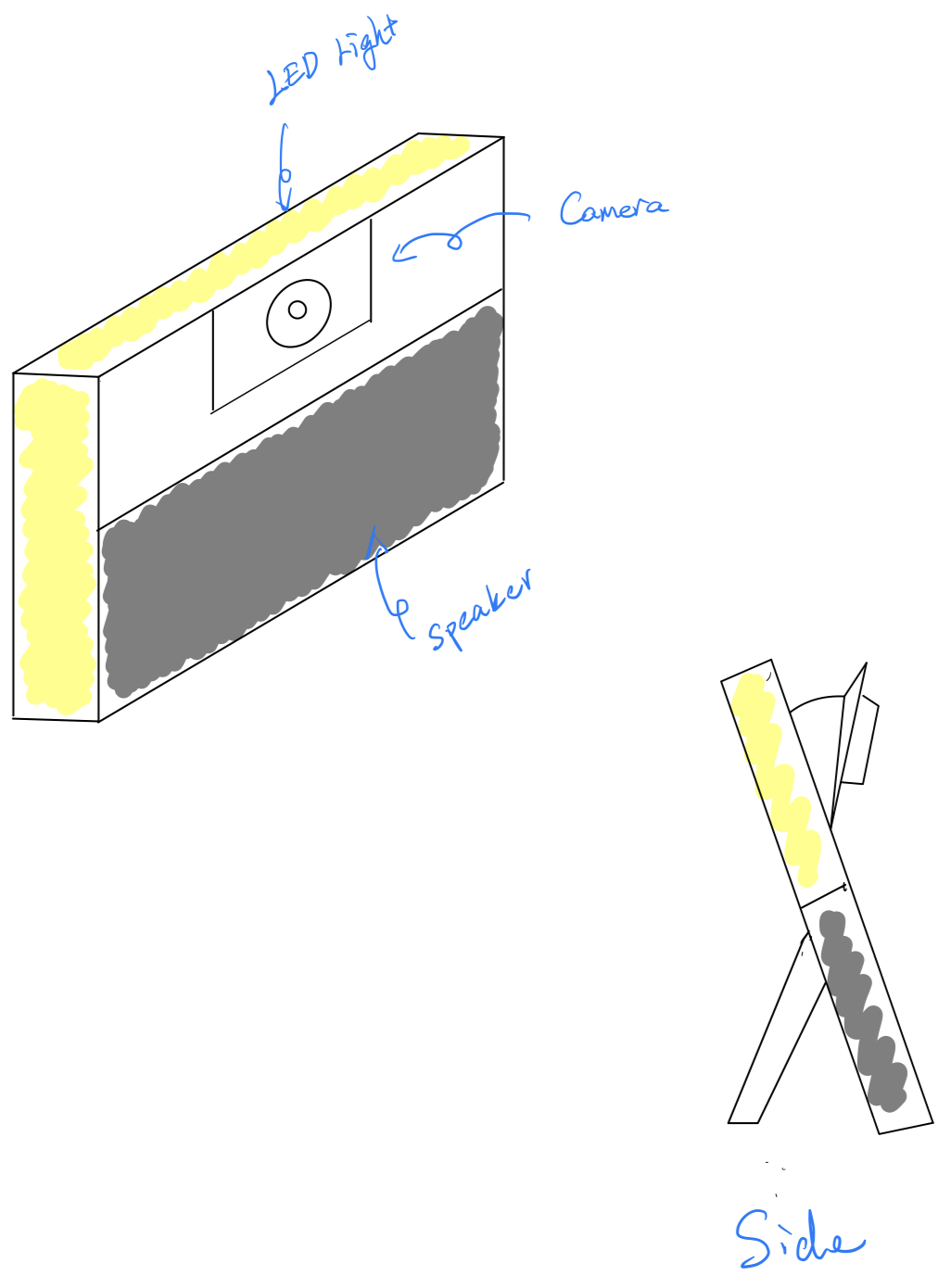
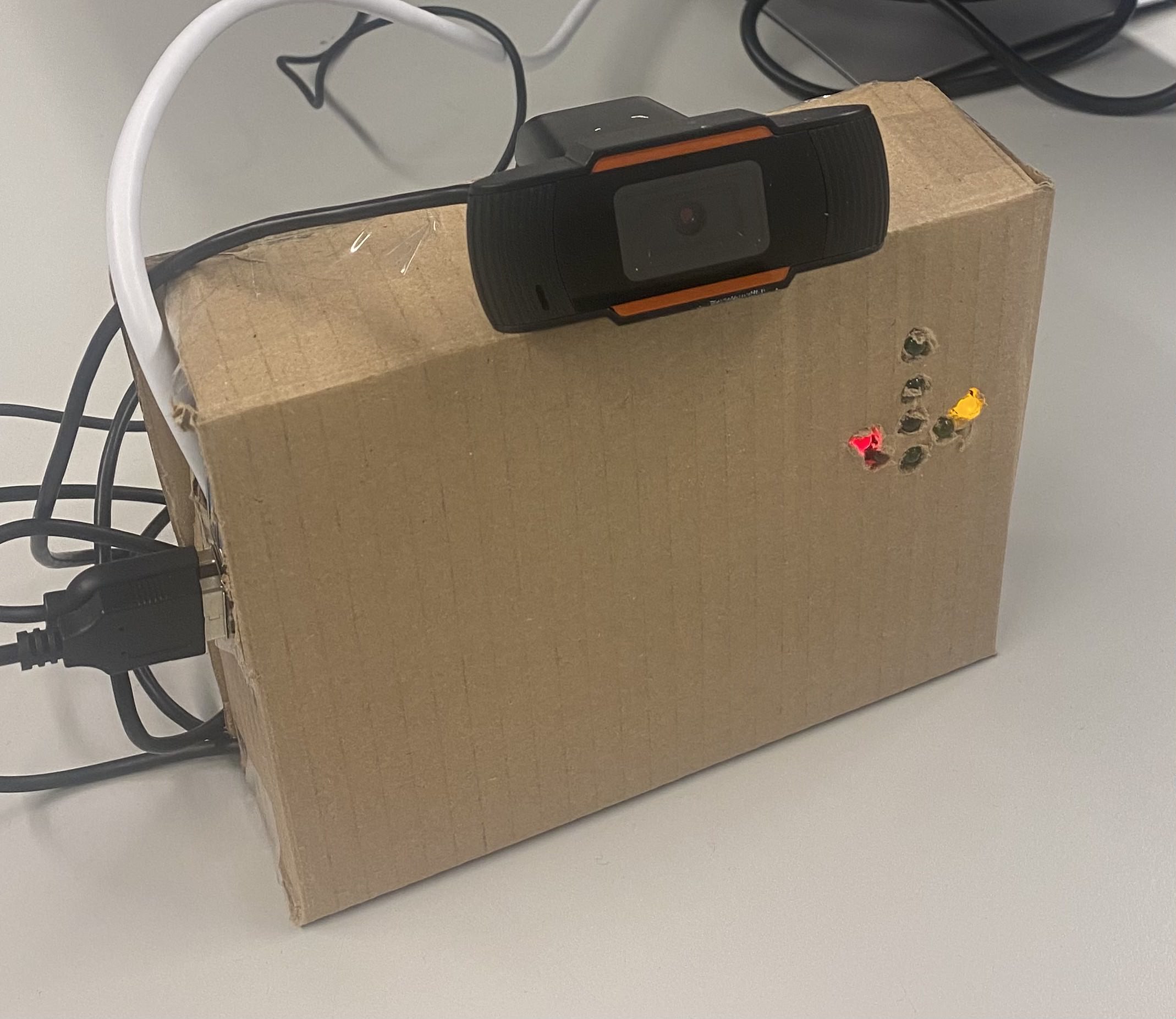
Innovative dining companion – a device designed to enhance your mealtime experience. With a built-in camera and practical algorithms, this product ensures you maintain your alertness and attention while enjoying your meals.
This system carefully monitors your engagement, recognizing your facial cues to measure your alertness. Once the algorithms detect any sign of distraction in your activity, it responds quickly, illuminating a soft LED glow while providing a gentle voice-over reminder through its embedded speaker. These activators are designed to guide you back to the present moment, encouraging you to focus on your meal.
Initial Design Component List
- Sensors
- Object Detection
- Camera - for seeing the face of the person eating.
- Any USB Webcam
- Raspberry Pi camera module + HDMI extension
- Ultrasonics - for detecting if someone is sitting in front of the device (might be nice for power drain as well). [This was scrapped due to time constraints.]
- HC-SR04: simple and precise enough for this task
- Camera - for seeing the face of the person eating.
- Object Detection
- Actuators
- Sound
- Speaker - for being able to make noises or play music.
- Any Bluetooth speaker.
- Speaker - for being able to make noises or play music.
- Light
- LEDs - for being able to attract attention back to the plate.
- To be able to use more than one LED on a GPIO, due to the current constraints on these pins, a separate circuit is needed, one with a transistor.
- LEDs - for being able to attract attention back to the plate.
- Sound
- Wires
- Jumper cables
- Female to male
- For testing proposes specifically on a breadboard
- Female to female
- From the output pins of the LED circuit, back to RPI
- Female to male
- Jumper cables
- Boards or computing units that this could work on
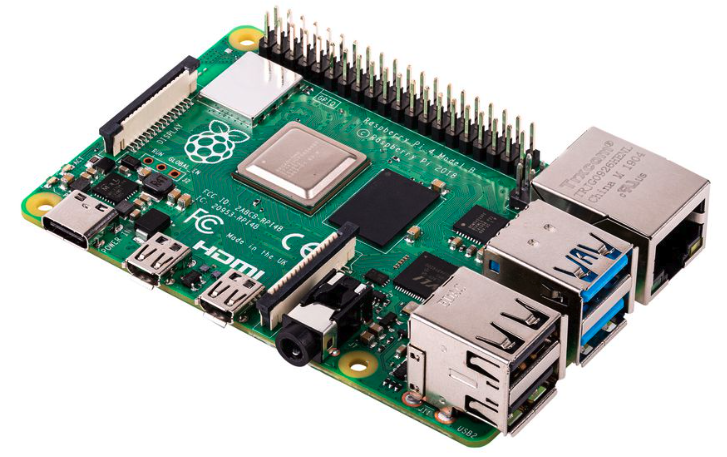
- RPI 4B:
- Has enough processing power
- Enough GPIO pins to drive different sensors
- A handy Bluetooth connection
- Is very well documented
- Pynq-Z2:
- More than enough processing power.
- Enough GPIO pins to drive different sensors
- Has an a 3.5 mm connector.
- RPI 4B:
- A power supply
- Any power bank.
- Batteries.
During the building and integration of the face tracking onto the board, we found out that due to the lack of documentation on the pynq-z2 it is quite hard to accomplish this. Due to the lack of time given by this course we opted using a RPI 4B, which has both processing and Bluetooth capabilities, guaranteeing a smooth transition between boards.
The components that are italicised are eventually used in the final product.
Product system description
Main operating device:
- Raspberry pi 4B
Actuators:
Camera
Face-recognition Algorithm
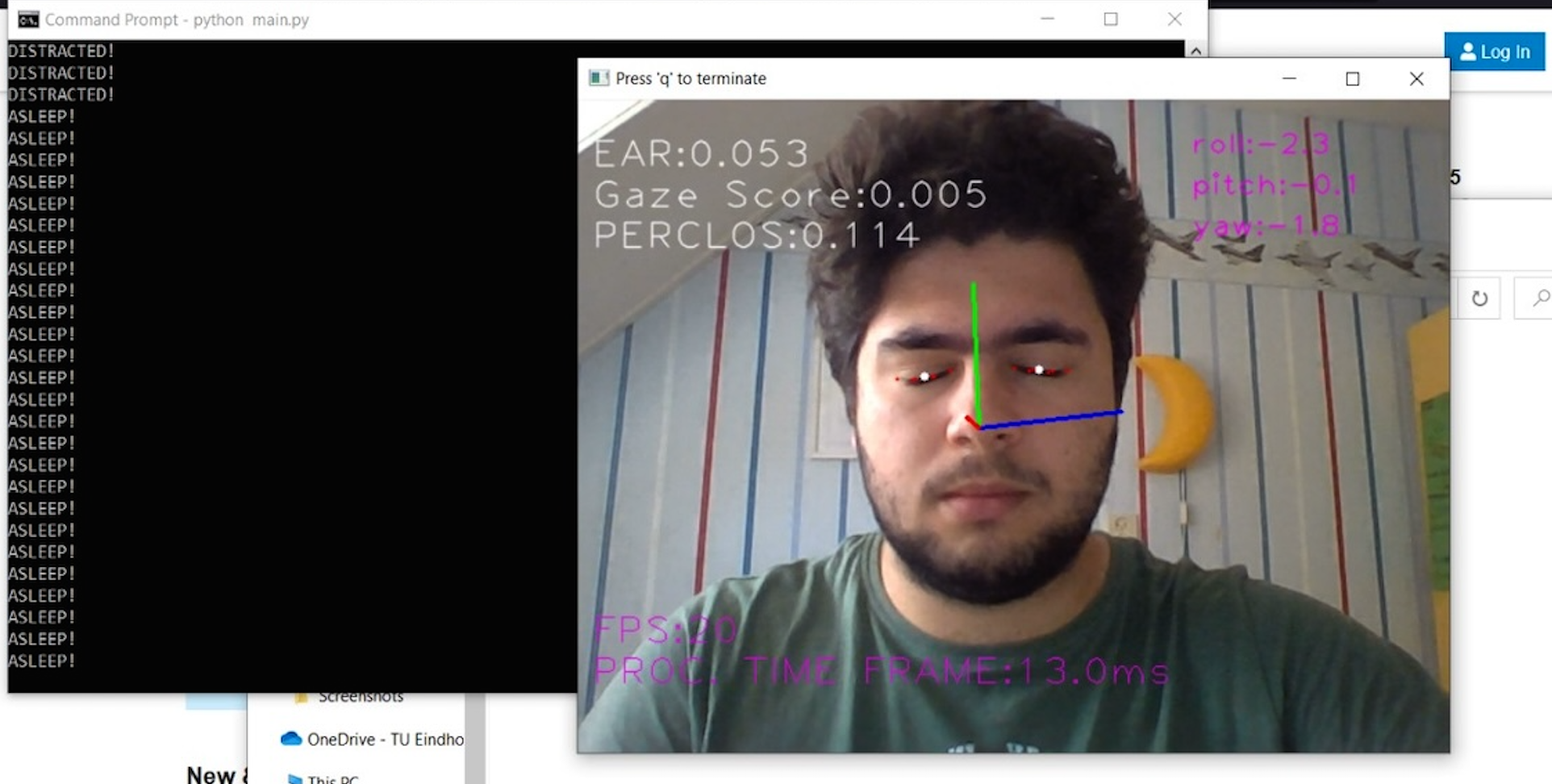
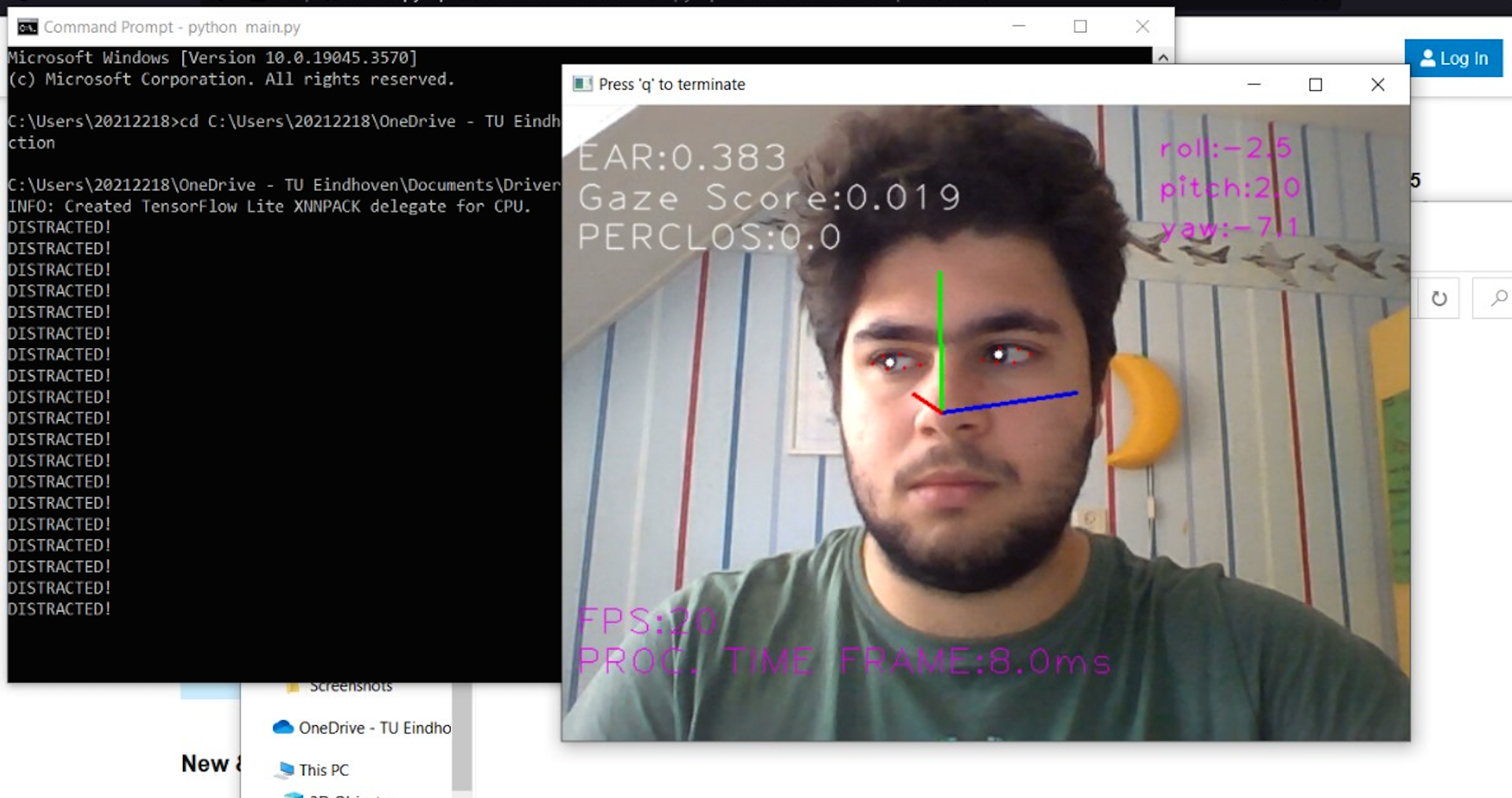
It is simple to use the device. one can place the device on a desk in which the user is having a meal and face the camera towards the user. Once the program is running, it will automatically monitor users face and eye movement and
we use face recognition algortihm to track facial movement and eye-movement to detect users state of activity. The algorithm
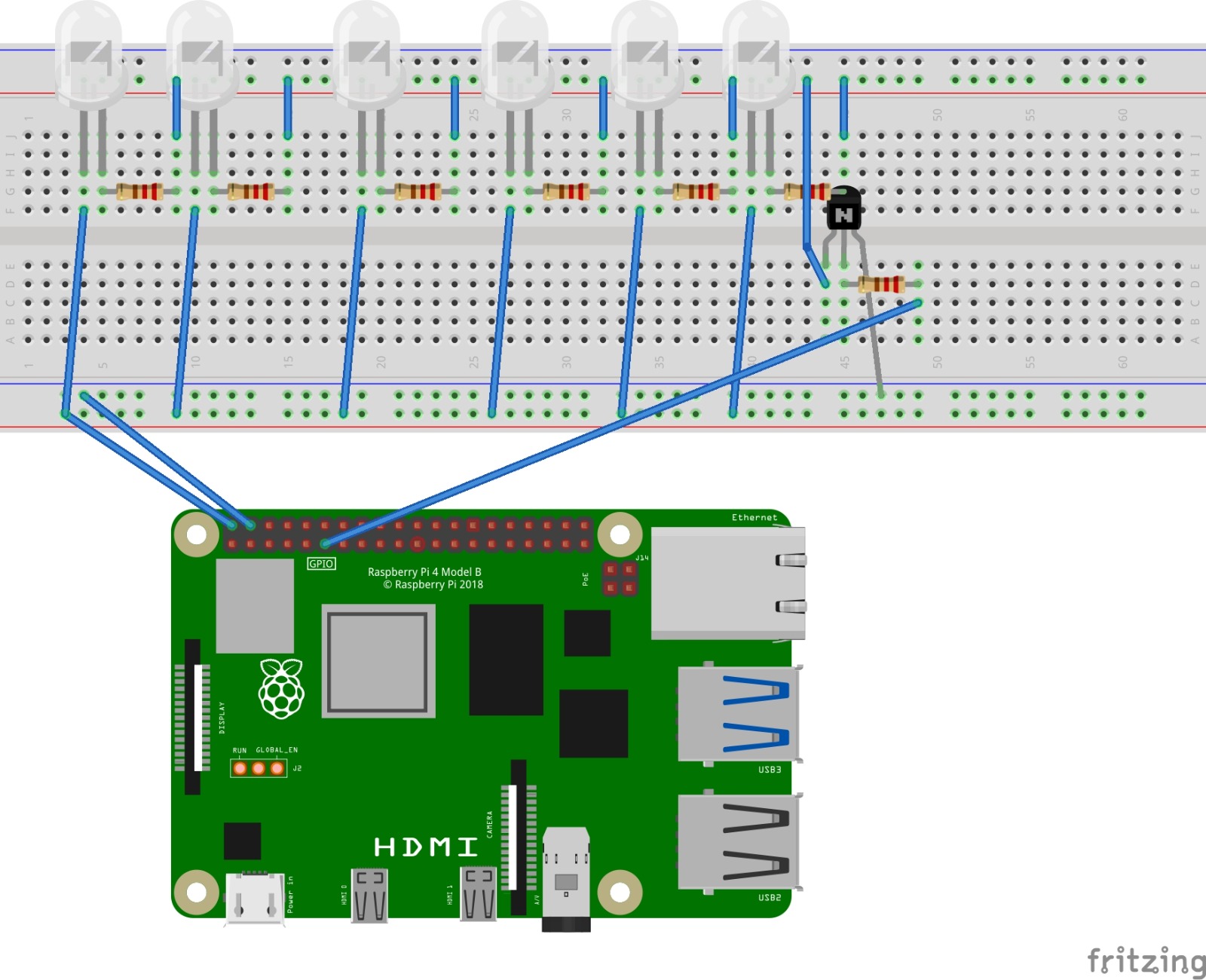
LEDs
For using any sensor or equipment that pulls more than 16 mA, a transistor/Mosfet should be used to not damage the board. This transistor ensures that by using the 5v supply on the board than enough current can be fed to the LEDs, for the limit on the 5v pin is 1A total.
By arranging the LEDs in the preferred manner and soldering them to a single sided pcb board to the transistor, and adding wires to the RPI. One can ensure a robust and functional way of adding LEDs, controlled by one GPIO pin on the RPI.
The resistor used at the gate pin of the transistor is to limit the current to the right level. The transistor can function as a switch up to its maximum gain.
Final Product
Test plan
Interviewee:
To test our device to see if it works and where/if it needs improvements we fist test it on ourselves. This is to see if the basic functions work and to see whether we can think of any improvements that can be made to optimize the performance of our device. Of course, testing on ourselves does not represent testing on our user group because we already know how the device is supposed to work. Therefore we have looked if we can find people with mild Alzheimer's on whom we can test our device. Unfortunately, we cannot find people with Alzheimer's that we know. To still be able to test our device on our user group, we have looked for people without Alzheimer's but who still can represent our user group. The problem which our device solves is loss of attention while eating. So our test group should be also coping with difficulty in maintaining attention. Therefore, our test group will be people with attention deficit hyperactivity disorder, better known as ADHD. These people commonly have some kind of eating difficulty due to their poor awareness of internal cues of hunger and satiety or fullness. The same goes for being easily distracted while eating and therefore struggling with finishing a meal which are the symptoms resembling dementia in terms of distraction during eating. We have found a few individuals we can use for testing our device.
Test setup:
For the test setup, every participant will sit at a table with a plate of food and the device in front of them. They will eat their meal while their device ensures that the person is not distracted and loses interest in eating. We will use different noises in each test to see which one performs best. Following the test, we will ask the test respondent the survey questions listed below to help us improve our device. Before completing this test, we ask them how they regularly eat so that we can determine whether there are enough distractions to observe what the difference is between eating with and without the device.
Test procedure:
- Provided yogurt to eat for testing
- Plays videos for them to watch
- Test until the user has finished the yogurt (~5min)
- Then, Ask survey questions
Survey questions:
- Did you have problems focusing while eating before?
- Did you get distracted while eating the yogurt during this testing?
- Does hearing the sound from the device alert you back to the meal? (scale: 1-5) If not, what improvement could be made?
- Did you think the sound was appropriate? If not, what sound would you prefer?
- Does the LED lighting from the device alert you back to the meal? (Scale: 1-5 ) If not, what improvement could be made?
- What do you think of the device in general? Do you think it will help for a user group who gets easily distracted like people with dementia?
User Interview
interviewee 1- Rudy
Interview questions
Did you have problems focusing while eating before?
- Yes
Did you get distracted while eating the yogurt during this testing?
- Don't think so, because I didn’t have problem finishing the yogurt
Does hearing the sound from the device alert you back to the meal? (scale: 1-5) If not, what improvement could be made?
- Definitely heard it, but 2 because i didn’t really know what that sound suppose to mean
Did you think the sound was appropriate? If not, what sound would you prefer?
- Sound was annoying. I prefer Softer sounds. The buzzer is definitely too harsh sound
Does the LED lighting from the device alert you back to the meal? (Scale: 1-5 ) If not, what improvement could be made?
- 1, did not affect me at all, didn’t really help me a lot, was not noticeable enough. Brighter, bigger, maybe adjust the sound and light so that we can make the light more noticeable compared to the sound.
What do you think of the device in general? Do you think it will help for a user group who gets easily distracted like people with dementia?
- While testing, the buzzer was ringing back of my mind, so I definitely have the device in my attention. I didn’t know what it was supposed to do to me, but it alerted me.
interviewee 2- Sid
Interview questions
Did you have problems focusing while eating before?
- Sometimes, usually when eating while playing with phone.
Did you get distracted while eating the yogurt during this testing?
- I got distracted by the sound more than the video (but it is because we didn’t tell them what the sound suppose to mean, which implies that the device actually attracted their attention)
Does hearing the sound from the device alert you back to the meal? (scale: 1-5) If not, what improvement could be made?
- I will give around 2.5.
Did you think the sound was appropriate? If not, what sound would you prefer?
- I think it reality does good job on attracting attention.
Does the LED lighting from the device alert you back to the meal? (Scale: 1-5 ) If not, what improvement could be made?
- 1, it wasn't noticeable enough
What do you think of the device in general? Do you think it will help for a user group who gets easily distracted like people with dementia?
- If you train the user how the device should be used, it might work.
interviewee 3- Minjin
Interview questions
Did you have problems focusing while eating before?
- Yes sometimes, depending on the situation.
Did you get distracted while eating the yogurt during this testing?
- I knew the testing environment beforehand(we told this user what the device suppose to do), so I did not get distracted because I was focusing on the yogurt most of the time
Does hearing the sound from the device alert you back to the meal? (scale: 1-5) If not, what improvement could be made?
- 3.5, it does brings my attention , improvement could be increase sound volume
Did you think the sound was appropriate? If not, what sound would you prefer?
- Increase sound volume
Does the LED lighting from the device alert you back to the meal? (Scale: 1-5 ) If not, what improvement could be made?
- 1, it didn’t really have any effect on bringing my attention. Maybe for improvement, you can use a screen instead of led lights
What do you think of the device in general? Do you think it will help for a user group who gets easily distracted like people with dementia?
- I don't think it will work for ADHD, because the device creates more distractions(sound, leds), but for dementia and Alzheimer patients, it might work. You could improve the visualization part of the device
State of the art
State of the art:
1. Smart plate:
- Focusses on weight loss
- Consist of a plate with different boxes with separate scales. An app that you need to take photo’s of your food with. And an AI that coaches you.
- Principle:
o Take photo of your food on the plate
o AI recognizes what is on your plate
o Scales detect how much
o Calculate the calories and macronutrients for you
o AI gives advise on what and how much to eat
- https://www.getsmartplate.com/
2. Non technology dinnerware
- Adaptive plates (deep ones, heating, suction cup, spill proof bowls)
- Adaptive utensils (big grip, non-slip surface, different design, special attachments)
- Adaptive cups
- https://www.healthproductsforyou.com/c-plates-and-bowls.html
3. SpoonTEK
- Enhances flavor
- How does it work?
o SpoonTEK generates a mild electric current to stimulate the tongue and alter taste. You cannot feel it but you do taste it.
- https://spoontek.com/
4. Liftware
- Smart spoon for hand tremors
- 2 different levels
o Reduce spilling from shaking
o Reduce spilling from tuning, twisting and shaking
- https://www.liftware.com/
Article summary
Natural history of hyperphagia and other eating changes in dementia [7]
The text discusses various dietary changes and challenges experienced by individuals with Alzheimer's or dementia. These changes include alterations in eating habits, malnutrition, dehydration, and a range of eating behavior disorders. Some individuals may show a decrease or increase in the amount eaten, changes in eating habits, food choice preferences (particularly for sweet foods), and even hyperphagia (excessive eating). Hyperphagia can lead to issues such as weight gain, eating dangerous foods, and constant food seeking. The article highlights the significance of these eating abnormalities, which can be a significant source of stress for caregivers and may lead to the need for institutional care. Weight loss is also a common concern among individuals with dementia and is associated with protein-energy malnutrition, increased mortality risk, morbidity, and a poor quality of life. Weight loss can start early in the disease's course and is related to cognitive decline. Additionally, the text mentions that certain factors, such as the severity of the disease and the emotional and material burden on family caregivers, can predict aversive eating behaviors in Alzheimer's disease. Sweet food preference and hyperphagia have been reported in a subset of patients with Alzheimer's disease.
Weight Loss and Nutritional Considerations in Alzheimer Disease [8]
This paper discusses some of the current methods of feeding assistance for people with Alzheimer's disease. These are: Caregiver Assistance: Caregivers can provide assistance during mealtime, such as sitting and chatting with the patient, giving specific instructions, and offering encouragement. In later stages, patients may have coordination difficulties, so serving finger foods can make eating easier. This approach has been shown to increase food intake. Texture Modification: As patients deteriorate, some may become intolerant of certain textures, so menu items may need to be prepared in softer or pureed forms to facilitate consumption. Meal Environment: Simplifying the mealtime environment, such as improving lighting, serving meals on individual plates, and scheduling nursing staff to assist during mealtimes, can improve food consumption and nutritional status. Nutritional Supplementation: This includes providing frequent snacks, fortified foods, and liquid supplements. Studies have shown that protein-energy supplementation can lead to weight gain and reduced mortality in undernourished individuals. Pharmacologic Agents: Some medications have been used to improve appetite or cause weight gain in patients with weight loss. However, their use is limited due to side effects, and further study is needed before clinical recommendations can be made. Tube Feeding: In cases where other interventions fail and patients have severe dementia, tube feeding may be considered. However, there is limited evidence to support its benefits, and it may increase the risk of infection and aspiration pneumonia.
Assessment of Perceived Attractiveness, Usability, and Societal Impact of a Multimodal Robotic Assistant for Aging Patients With Memory Impairments
[9]
This study aims to assess the clinical application of a robotic assistant for patients with mild cognitive impairments (MCI) and Alzheimer's Disease. Testing was conducted with the prototype version of the Robotic Assistant for MCI Patients at Home (RAMCIP) in a controlled environment, involving 18 elderly participants (10 healthy and 8 with MCI). Participants performed various tasks facilitated by RAMCIP, such as medication intake, hazard prevention, and social interaction. No significant differences were observed between the groups in terms of perceived attractiveness, usability, or social impact, with high assessments for attractiveness and social impact but neutral feedback on usability due to the limited interaction time. The study emphasizes the increasing need for support for the aging population, particularly those experiencing memory impairments. It highlights the potential role of robotic assistants in aiding caregivers and enhancing the independence and security of elderly individuals. The research methodology follows a user-centric approach, involving medical professionals, caregivers, and end-users in the evaluation process. The robot's design and functionalities have been adjusted based on user feedback. The RAMCIP prototype offers support in various aspects, including reacting to potential hazards, assisting with cooking, monitoring medication intake, providing cognitive stimulation, and maintaining social connections through multimodal communication. The study focuses on assessing the acceptability, usability, and social impact of the RAMCIP prototype among users. Standardized questionnaires and surveys are used for evaluation, with positive results in terms of acceptance and social impact, but neutral opinions on usability. In summary, this study evaluates the clinical application of a robotic assistant for individuals with cognitive impairments, emphasizing user perception and social impact, and aims to improve the robot's usability and acceptance among the target population.
The efficacy of cognitive prosthetic technology for people with memory impairments: A systematic review and meta-analysis
[10]
The purpose of this paper was to provide a detailed review of the quality of studies that have investigated memory orthotic technology with people with memory problems and to relate these findings to the different categories of technology. Studies testing cognitive orthotic devices with adults with any brain injury, trauma or neurological/degenerative disease. The NeuroPage has been highlighted in previous reviews as being the technology with the most evidence for its efficacy. Combining portable and non-portable PDA’s has excellent prospects for patients with memory impairment due to surgeries. However, in the case of degenerate diseases, such as Alzheimer’s, the benefits have still to be researched. Furthermore Future research should aim to establish whether or not there is a benefit to using technology instead of non-technological reminders, such as calendars.
Easily accessible and cheap smartphones are also a promising development in supporting patient with memory impairment. Touchscreen makes it more accessible for elderly users instead of a device with buttons. Also smartphones or portable tablets have the advantage that they are highly adaptable to personal preferences. On the other hand, using a smartphone or tablet device as a reminder may be less effective because of the number of different functions it provides and because they will not always be within the vicinity of the user.
Micro-prompting devices another promising development in memory impairment help. The details of the devices is not discussed in the paper (find other source for micro prompting devices in SCED studies). While prospective prompting devices and micro-prompting devices differ in the type of memory performance they are designed to aid, these findings suggest that if applied correctly both could be useful for memory impaired patients.
Eating Behavior in Aging and Dementia: The Need for a Comprehensive Assessment [11]
- Eating behavior changes with aging, influenced by physiological, psychological process, and social factors.
- These changes encompass food choice, eating habits, and dietary intake.
- Dietary behavior, such as the Mediterranean diet, can impact the risk of age-related pathologies like dementia.
- Dementia can be associated with significant eating behavior modifications, including weight loss and dietary changes.
- Screening tools like the Mini Nutritional Assessment (MNA) and Simplified Nutritional Appetite Questionnaire (SNAQ) help assess eating behavior in aging individuals, while tools like the Eating Behavior Scale (EBS) and Cambridge Behavioral Inventory (CBI) are useful in identifying symptoms of dementia.
- Management of eating behavior in aging and dementia involves a combination of strategies, including dietary adjustments, environmental modifications, and caregiver support.
- Alzheimer's disease, which accounts for 60% of all cases of dementia, introduces the problem of over and under eating. Due to the forgetfulness that comes with it.
- As this disease progresses dysfunctions like swallowing tend to worsen. This together with general changes, can make nutritional intake quite the challenge
- Right now is combatted by caregivers or the patients will have to be in a nursery home, improving regularity.
- Weight loss has always been a main symptom of Alzheimer's.
Eating habits and behaviors of older people: Where are we now and where should we go? [12]
- Eating habits influenced by social and psychological changes. Financial, loneliness, depression
- Macronutrients: protein, carbohydrates, lipids
- Many older adults avoid consuming animal protein because they find it difficult to chew and swallow, because of the age-related decline in their sense of smell and taste, or because of health concerns about their intake of cholesterol and saturated fat.
- Animal sources provide on average 60% of their total protein intake, the greatest part of that being in a meal
- Reviews suggest that older people should consume 25–30 g of high-quality protein at each meal in order to achieve the maximum anabolic response
- Older people are more prone to vitamin B12 deficiency due to insufficient intake of animal foods, such as meat, which are good sources of B12. Results from a recent review estimated that 16% and 19% of older men and women respectively have intakes below the average requirement of the vitamin, with mean daily intakes of 6.4 and 5.1 micrograms respectively
- Author suggested a couple diet programs such as DASH, MIND, Okinawa diet to tackle these issues.
Changes in appetite, food preference, and eating habits in frontotemporal dementia and Alzheimer’s disease [13]
- Frontotemporal dementia (FTD) is characterized by progressive focal atrophy in the frontal or anterior temporal lobes and is associated with various non-Alzheimer pathologies.
- FTD can manifest with predominantly frontal involvement, known as frontal variant FTD (fv-FTD), leading to behavioral changes such as loss of insight, impulsivity, mood changes, and altered eating behaviors.
- Research comparing FTD subgroups and Alzheimer's disease in terms of eating behavior changes has been limited but is crucial for both clinical and theoretical understanding.
- This study used a caregiver questionnaire to investigate eating behavior changes in FTD and Alzheimer's disease, aiming to determine their frequency, sequence of development, and variations among FTD subtypes.
- Results showed that eating behavior changes were more common in both FTD subgroups compared to Alzheimer's disease, with alterations in appetite and food preferences being significant features in FTD, while Alzheimer's disease mainly exhibited loss of appetite.
An open-ended question: Alzheimer’s disease and involuntary weight loss: which comes first? [14]
- Involuntary weight loss (IWL) and malnutrition have been observed in Alzheimer's disease (AD) patients for many years.
- Clinically relevant IWL is typically defined as a loss of at least 5% of usual body weight over 6-12 months.
- IWL can result from various factors, including disturbances in calorie intake, absorption, utilization, and loss.
- Malnutrition in the elderly, including AD patients, is considered a geriatric syndrome with multiple contributing factors.
- Early evaluation of IWL in elderly patients is crucial to prevent malnutrition, which can lead to complications.
- Nutritional status and dementia are interconnected, with IWL being common in AD cases.
- The relationship between AD and IWL is complex and may involve bidirectional causality.
- AD-related brain changes can impact food intake regulation, leading to IWL.
- IWL may precede the clinical onset of AD and contribute to its progression.
- Strategies for preventing IWL in AD patients include nutritional assessment, caregiver support, and oral nutritional supplementation.
Eating disorders in the elderly[15]
The article looks at eating disorders in people above 50.
- Eating disorders in elderly are a serious concern.
- 88% of the cases were female.
- 80% of the cases were anorexic.
- Depression is seen a lot of times in combination with eating disorders.
- Only 42% were treated successfully and 21% died with their disorder as cause.
Factors affecting independence in eating among elderly with Alzheimer's disease[16]
The article uses regression techniques to research the factors that affect people with Alzheimer disease the most in eating independently.
- The beginning of a meal was an important difficulty.
- It is of importance to find ways to help people with Alzheimer Disease to begin eating, if they want to remain independent.
Further edits and findings from this paper:
- This paper also mentions how people with moderate dementia (based on the Clinical Dementia Rating (CDR)) are still quite independent regarding eating for example.
- It is noted in this text that even during later stages the will to feed one self (autonomous) is very much present.
- Also some problems are nicely detailed (see next page):
- Clearly early stage dementia is not the target area or at least not complete enough for except from dysphagia, it seems the problems with feeding is quite minimal ~10% ()
- The study had 324 participants
- Major Findings: This paper single-handedly shows the different problems a person with dementia faces, the list can be found in the paper, but a few notable ones are presented here:
- Difficulty in beginning the meal.
- Difficulty in recognizing the total amount of food provided
- Difficulty in maintaining attention while eating
- Difficulty in maintaining alertness while eating
- As seen in the tables of this paper, these difficulties are most present in the later stages of dementia, this shifts our focus group towards mild levels of dementia.
Eating disorders in elderly: Clinical implications[17]
The article stresses the importance of taking eating disorders seriously in the elderly population.
- Psychological & Social Factors play a sizable role.
- There are several Psychiatric aspects to eating disorders in elderly.
Treatment of eating disorders in older people: a systematic review[18]
The article looks systematically at the treatment of elderly with eating disorders.
- The majority of cases is female (85%)
- 84.6% ate was identified with anorexia nervosa.
- 95% were treated, where 52% were treated with a hospital-based treatment.
- 80% improved during treatment, but the other 20% relapsed or died.
- Hard to make conclusions as results were very different.
Eating Behaviors and Dietary Changes in Patients With Dementia[19]
- Malnutrition or undernourishment resulting from insufficient food intake is reported in up to 85% of nursing home residents
- Changes in eating in dementia include a decrease or increase in amount eaten (with or without weight changes), a change in eating habits (for instance, a change in the frequency of eating, playing with food, and improper or no use of utensils), a change in food choice (most commonly a predilection toward sweet foods), and pica (persistent ingestion of non-nutritive substances).
- A peculiar change is represented by hyperphagia that can be a serious aspect for several reasons, for example, weight gain, eating dangerous foods, and continual searching for food.
- The caregivers indicated that “forgetting” was the first and most common eating characteristic exhibited by the patients, which contributed to overeating.
- Mentions a few types of dementia, with a good visualization, showing the different symptoms come with different forms of dementia.
- As with many areas of intimate care, such as bathing and attending to toilet needs, there is relatively little research on individualized interventions about eating in persons with dementia, particularly when it is carried out at home.
Feeding and dementia: a systematic literature review[20]
- This paper discusses what is already known about this topic
- Older people with dementia experience difficulty with feeding.
- Feeding difficulty is associated with decline in cognitive function and with physical decline.
- There is a lack of research into interventions aimed at helping older people with dementia to feed.
- What this paper adds
- Intervention studies of feeding and dementia lack statistical power.
- There are no standardized interventions or outcomes across intervention studies of feeding and dementia.
- Studies of interventions to alleviate feeding difficulty in dementia do not account adequately for confounding factors.
- Tldr; It is basically an entire document discussing the interventions that have been researched.
- However these "interventions" are more so techniques than technology, but because they do help with feeding for the elderly with forms of dementia, it still falls inside the scope of our research.
- A newer more modern version of this is also made, as can be seen in: "Effectiveness of interventions on feeding difficulties among people with dementia: A systematic review and meta-analysis"[21]
Exploring perception of eating with dementia: Findings from a massive open online course[22]
- Basically a nice paper to get some insight to what elderly with dementia think of the help that is provided already. This data is from an online course called Understanding Dementia, filled in by participants mostly over the age of 50, and also caregivers.
- This paper finds out how and what the elderly think about the current perceptions of the care given/received when eating.
- So not really relevant to coming up with the idea of an intervention itself, but it does add insight in how they think about the care right now, and give some USErs restraints.
Eating and Drinking - Alzheimer's Society[23]
- People with dementia often have physical difficulties including hearing and sight loss that can also cause problems with eating and drinking. This webpage, is more about general information for elderly/people with Alzheimer's. The findings of this page relevant for us can be summarized as follows:
- It is a good idea to include later stages of dementia into our group and focus on specifics, as their problems are more apparent.
- As dementia progresses, the person is likely to need more support to meet their needs. While eating a balanced diet is recommended, sometimes it is more important to make sure they are eating enough, even if that means eating unhealthy foods. They may also need more support with drinking.
- Diets seem quite unsustainable as at a certain point getting food in is a priority over considering the macronutrients.
Dementia and Dysphagia[24]
- “Durnbaugh, Haley, and Roberts found that by eliminating distractions during mealtime, individuals with dementia improved their nutrition and caloric intake. They recommend removing condiments from meal trays and keeping desserts out of sight until the end of the meal. Avoid interruptions during mealtimes and provide encouragement to self-feed."
- The rest of the paper, mostly discusses dysphagia itself, which is interesting in and of itself, however falls outside of our problem statement.
Assessing Problem Feeding Behaviors in Mid-Stage Alzheimer's Disease[25]
- This paper also discusses problems that arise when a client with Alzheimer's/Dementia tries to eat.
- For this paper the clients were observed at meal-times by gerontologic clinic nurse specialists, and noted their findings. These findings where filled in a form that was predetermined
- The problems that arose can be found in tables, in our case common mealtime problems are a major point, so a few will be listed here:
- Distracted from eating
- Plays with food
- Stares without eating
- Some citations that prove to be helpful regarding our problem statement:
- “Clients were often distracted from eating. Distractions were abundant: noise, other clients, staff engaging in non-mealtime activities, such as taking vital signs or giving medications. Clients stopped eating for significant periods because of distractions.”
- After about a third to a half of the meal was consumed, clients resisted finishing the meal, often stating, "No more," or "I'm finished." If staff approached clients immediately when they stopped eating, the subjects appeared to become more resistant. If there was a short interval before staff approached clients, they often would begin to eat again when requested.
Factors affecting the appetites of persons with Alzheimer's disease and mild cognitive impairment[26]
- Some helpful citations from this paper:
- "The present study showed that Vitality Index, number of comorbidities, and the use of antidementia and psychotropic drugs were correlated with appetite loss among individuals with AD, whereas difficulty maintaining attention while eating and depression were commonly associated with appetite loss in both AD and MCI."
- " "Difficulty in maintaining attention while eating” means that a person cannot pay attention during meals, and is distracted by sounds, moving people and other factors. Because the present study was cross-sectional, we could not conclude whether difficulty in maintaining attention while eating could cause appetite loss, but difficulty in maintaining attention while eating would be one of the indicators of appetite loss."
Cognitive Distraction at Mealtime Decreases Amount Consumed in Healthy Young Adults: A Randomized Crossover Exploratory Study[27]
- This paper compares the food intake (macronutrient level & sheer amount) of young adults, while focused and distracted and lists it's findings. Useful findings from this paper:
- “When distracted, individuals consumed significantly less than when they were not distracted”
- It appears that the influence of distraction is different based on what type of distraction is used.
- They state a difference between mindless eating and distracted eating, the difference being:
- “To be considered a distracted eating episode, however, there must be a conscious decision to consume the meal, but when the actual consumption begins, the individual's attention is actively diverted.”
- “In a mindless eating episode, an individual does not make a deliberate choice to begin eating.”
- This makes us focus more specifically on distracted eating behaviour.
- Distracted eating is often also linked to snacking more, due to forgetting the meal however this paper denotes the following
- “This decrease in memory did not, however, result in an increase in snack consumption as was previously hypothesized.”
Personal Efforts
| Name | Time Spent | Breakdown |
|---|---|---|
| YooungGi Park | 8.5 | lecture, group meeting, subject research, wiki edit(Milestones) |
| Zabiollah Amiri | ||
| Thomas Paul Smids | ||
| Name | Time Spent | Breakdown |
|---|---|---|
| YooungGi Park | 9 | Tutor, group meeting, 4 article research & summary, first conceptual design |
| Zabiollah Amiri | Group meeting, 5 articles summarized, first conceptual design | |
| Thomas Paul Smids | ||
| Name | Time Spent | Breakdown |
|---|---|---|
| YooungGi Park | 8 | Tutor, group meeting, research on problems for early dementia patients and eating disorder, functional requirements |
| Zabiollah Amiri | Group meeting, 5 articles summarized, first conceptual design | |
| Thomas Paul Smids | ||
| Name | Time Spent | Breakdown |
|---|---|---|
| YooungGi Park | 8 | Tutor, group meeting, concept design, sketch initial design |
| Zabiollah Amiri | Group meeting, 5 articles summarized, first conceptual design | |
| Thomas Paul Smids | ||
| Name | Time Spent | Breakdown |
|---|---|---|
| YooungGi Park | 11 | Tutor, group meeting, research development enviornment for pynq board, coding for actuators on pynq board, create cardboard design |
| Zabiollah Amiri | Group meeting, 5 articles summarized, first conceptual design | |
| Thomas Paul Smids | ||
| Name | Time Spent | Breakdown |
|---|---|---|
| YooungGi Park | 14 | Tutor, group meeting, continue working with the product (coding & pynq board), search users for testing, editing wiki |
| Zabiollah Amiri | Group meeting, 5 articles summarized, first conceptual design | |
| Thomas Paul Smids | ||
| Name | Time Spent | Breakdown |
|---|---|---|
| YooungGi Park | 13 | Tutor, group meeting, Switching to Raspberry Pi 4, user testing, presentation preperation |
| Zabiollah Amiri | Group meeting, 5 articles summarized, first conceptual design | |
| Thomas Paul Smids | ||
| Name | Time Spent | Breakdown |
|---|---|---|
| YooungGi Park | 7 | Presentation, group meeting, editing wiki |
| Zabiollah Amiri | Group meeting, 5 articles summarized, first conceptual design | |
| Thomas Paul Smids | ||
References
- ↑ Ludwig DS. Lifespan Weighed Down by Diet. JAMA. 2016;315(21):2269–2270. doi:10.1001/jama.2016.3829
- ↑ Tamura, B. K., Masaki, K. H., & Blanchette, P. (2007). Weight loss in patients with Alzheimer's disease. Journal of nutrition for the elderly, 26(3-4), 21–38. https://doi.org/10.1300/j052v26n03_02
- ↑ Edahiro, A., Hirano, H., Yamada, R., Chiba, Y., Watanabe, Y., Tonogi, M., & Yamane, G. (2012). Factors affecting independence in eating among elderly with Alzheimer’s disease. Geriatrics & Gerontology International, 12(3), 481–490. https://doi.org/10.1111/j.1447-0594.2011.00799.x
- ↑ Edahiro, A., Hirano, H., Yamada, R., Chiba, Y., Watanabe, Y., Tonogi, M., & Yamane, G. (2012). Factors affecting independence in eating among elderly with Alzheimer’s disease. Geriatrics & Gerontology International, 12(3), 481–490. https://doi.org/10.1111/j.1447-0594.2011.00799.x
- ↑ What are the signs of Alzheimer’s disease? (n.d.). National Institute on Aging. https://www.nia.nih.gov/health/what-are-signs-alzheimers-disease#:~:text=For%20most%20people%20with%20Alzheimer's,30s%2C%20although%20this%20is%20rare.
- ↑ Symptomen alzheimer | Alzheimer Nederland. (n.d.). Alzheimer Nederland. https://www.alzheimer-nederland.nl/dementie/soorten-vormen/ziekte-van-alzheimer/symptomen
- ↑ Natural history of hyperphagia and other eating changes in dementia. (1998). PubMed. https://doi.org/10.1002/(sici)1099-1166(1998100)13:10
- ↑ Smith, K., & Greenwood, C. E. (2008). Weight loss and nutritional considerations in Alzheimer disease. Journal of Nutrition for the Elderly, 27(3–4), 381–403. https://doi.org/10.1080/01639360802265939
- ↑ Gerłowska, J., Skrobas, U., Grabowska-Aleksandrowicz, K., Korchut, A., Szklener, S., Szczęśniak-Stańczyk, D., Tzovaras, D., & Rejdak, K. (2018). Assessment of perceived attractiveness, usability, and societal impact of a multimodal robotic assistant for aging patients with memory impairments. Frontiers in Neurology, 9. https://doi.org/10.3389/fneur.2018.00392
- ↑ Jamieson, M., Cullen, B., McGee-Lennon, M., Brewster, S., & Evans, J. J. (2014). The efficacy of cognitive prosthetic technology for people with memory impairments: a systematic review and meta-analysis. Neuropsychological Rehabilitation, 24(3–4), 419–444. https://doi.org/10.1080/09602011.2013.825632
- ↑ Fostinelli, S., De Amicis, R., Leone, A., Giustizieri, V., Binetti, G., Bertoli, S., Battezzati, A., & Cappa, S. F. (2020). Eating Behavior in Aging and Dementia: the need for a Comprehensive assessment. Frontiers in Nutrition, 7. https://doi.org/10.3389/fnut.2020.604488
- ↑ Yannakoulia, M., Mamalaki, E., Anastasiou, C. A., Mourtzi, N., Lambrinoudaki, I., & Scarmeas, N. (2018). Eating habits and behaviors of older people: Where are we now and where should we go? Maturitas, 114, 14–21. https://doi.org/10.1016/j.maturitas.2018.05.001
- ↑ M Ikeda, J Brown, A J Holland, R Fukuhara, J R Hodges (2001).Changes in appetite, food preference, and eating habits in frontotemporal dementia and Alzheimer’s disease. J Neurol Neurosurg Psychiatry 2002;73:371–376 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1738075/pdf/v073p00371.pdf
- ↑ Inelmen, E. M., Sergi, G., Coin, A., Girardi, A., & Manzato, E. (2010). An open-ended question: Alzheimer’s disease and involuntary weight loss: which comes first? Aging Clinical and Experimental Research, 22(3), 192–197. https://doi.org/10.1007/bf03324796
- ↑ Lapid, M. I., Prom, M. C., Burton, M. C., McAlpine, D. E., Sutor, B., & Rummans, T. A. (2010). Eating disorders in the elderly. International Psychogeriatrics, 22(4), 523–536. https://doi.org/10.1017/s1041610210000104
- ↑ Edahiro, A., Hirano, H., Yamada, R., Chiba, Y., Watanabe, Y., Tonogi, M., & Yamane, G. (2012). Factors affecting independence in eating among elderly with Alzheimer’s disease. Geriatrics & Gerontology International, 12(3), 481–490. https://doi.org/10.1111/j.1447-0594.2011.00799.x
- ↑ Cotet, C. (2023, March 8). EATING DISORDERS IN ELDERLY: CLINICAL IMPLICATIONS - Journal of Evidence-Based Psychotherapies. Journal of Evidence-Based Psychotherapies. http://jebp.psychotherapy.ro/vol-xix-no-2-2019/eating-disorders-in-elderly-clinical-implications/
- ↑ Mulchandani, M., Shetty, N., Conrad, A. M., Muir, P., & Mah, B. (2021). Treatment of eating disorders in older people: a systematic review. Systematic Reviews, 10(1). https://doi.org/10.1186/s13643-021-01823-1
- ↑ Cipriani, G., Carlesi, C., Lucetti, C., Danti, S., & Nuti, A. (2016b). Eating behaviors and dietary changes in patients with dementia. American Journal of Alzheimers Disease and Other Dementias, 31(8), 706–716. https://doi.org/10.1177/1533317516673155
- ↑ Watson, R., & Green, S. (2006b). Feeding and dementia: a systematic literature review. Journal of Advanced Nursing, 54(1), 86–93. https://doi.org/10.1111/j.1365-2648.2006.03793.x
- ↑ Chang, H., Spencer, J., Ho, M., Kasa, A. S., Ataiza, C., Lambert, K., & Chang, C. (2023b). Effectiveness of interventions on feeding difficulties among people with dementia: A systematic review and meta‐analysis. Australasian Journal on Ageing. https://doi.org/10.1111/ajag.13192
- ↑ Goodwin, I., Lea, E., Bindoff, A., & Doherty, K. (2022b). Exploring perceptions of eating with dementia: Findings from a massive open online course. Appetite, 177, 106126. https://doi.org/10.1016/j.appet.2022.106126
- ↑ Eating and drinking. (n.d.). Alzheimer’s Society. https://www.alzheimers.org.uk/get-support/daily-living/eating-drinking
- ↑ Easterling, C., & Robbins, E. (2008). Dementia and dysphagia. Geriatric Nursing, 29(4), 275–285. https://doi.org/10.1016/j.gerinurse.2007.10.015
- ↑ Durnbaugh, T., Haley, B., & Roberts, S. (1996). Assessing problem feeding behaviors in mid-stage Alzheimer’s disease. Geriatric Nursing, 17(2), 63–67. https://doi.org/10.1016/s0197-4572(96)80170-4
- ↑ Suma, S., Watanabe, Y., Hirano, H., Kimura, A., Edahiro, A., Awata, S., Yamashita, Y., Matsushita, K., Arai, H., & Sakurai, T. (2018). Factors affecting the appetites of persons with Alzheimer’s disease and mild cognitive impairment. Geriatrics & Gerontology International, 18(8), 1236–1243. https://doi.org/10.1111/ggi.13455
- ↑ Liguori, C., Nikolaus, C. J., & Nickols‐Richardson, S. M. (2020). Cognitive Distraction at Mealtime Decreases Amount Consumed in Healthy Young Adults:A Randomized Crossover Exploratory Study. Journal of Nutrition, 150(5), 1324–1329. https://doi.org/10.1093/jn/nxaa022